Jeff Thekkekara, OMS-IV, Kansas City University of Medicine and Biosciences
The discovery of the electrocardiogram (ECG) by the Dutch physiologist, Dr. Wilhelm Einthoven, would eventually win him the Nobel Prize in 1924, but he could not have done so without the knowledge that came before him. For example, Dr. Carlo Matteucci’s discovery that an electrical current is produced with each heart beat and Gabriel Lippmann’s invention of the capillary electrometer. These inventions and discoveries formed a foundational knowledge that led to Dr. Einthoven’s work and the modern iteration of the ECG that has helped many patients since. I aim to provide further knowledge about one aspect of the ECG, namely the T-wave inversions, which is commonly encountered in hospitals and emergency departments worldwide.
The T-wave normally occurs after the QRS complex and represents ventricular repolarization. The T-wave is normally inverted, or negative, in lead aVR and variable in leads III, aVL, aVF, and V1. In children who may have a more dominant right ventricle, the T-wave can be inverted in leads V1-3 (Figure 1). This is a normal finding that generally disappears with aging.
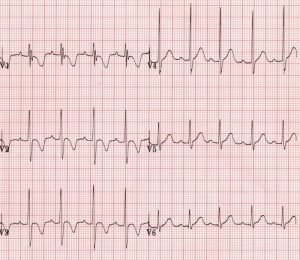
Figure 1: Pediatric T waves
Another normal finding of T-wave inversions can be seen in the young Afro-Caribbean female population. Persistent Juvenile T-waves are usually asymmetric and shallow (<3mm) and limited to V1-3 as well (Figure 2). This pattern may persist into adulthood.

Figure 2: Persistent Juvenile T waves
The final important normal occurrence of T-wave inversions occurs transiently in the athletic heart. In a sample of cross country skiers, the image below demonstrates how variable their QRS and T waves can appear in leads V1-3 (Figure 3) throughout exercise. This is a rare occurrence affecting about 3% of patients.

Figure 3: Athletic Heart
Now, our discussion will move on to transient T-wave inversions that are pathologic. The most common cause of pathologic T-wave inversions is myocardial ischemia. In cases of ischemia, the inversion can be classified as dynamic, which occurs acutely, or fixed, which can indicate prior infarction. The waves are narrow, sharp, and symmetric (Figure 4). Note that even a fixed T-wave inversion generally persists only for a matter of weeks, and thus it would still be considered a transient etiology. Even Coronavirus can manifest as acute coronary syndrome. These cases can present with T-wave inversions or depression among other ECG abnormalities.
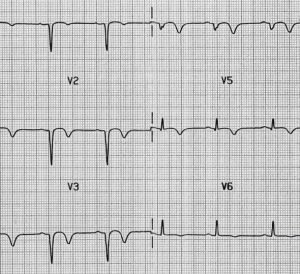
Figure 4: Myocardial Ischemia
Another acute phenomenon that causes T-wave inversions is a massive pulmonary embolism. When an embolus is large enough and gets lodged in the blood vessels, it can cause a right heart strain pattern that mimics right ventricular hypertrophy. This *high yield* ECG is memorized by medical student with the phrase: “SIQIIITIII” because it features an S wave in lead I, a Q wave in lead III, and a T-wave inversion in lead III, as noted in the image below (Figure 5).
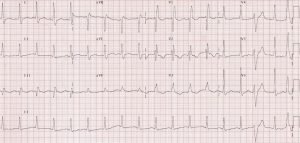
Figure 5: Massive Pulmonary Embolism
The next cause of transient T-wave inversions is unique in that if the patient is closely followed with serial ECGs the change can be delineated. Usually following a viral infection, acute pericarditis is an inflammatory condition that can manifest with tachycardia or dyspnea. The general course of acute pericarditis is as follows (Figure 6):
Stage 1 (from the first week): widespread ST elevations and PR depression
Stage 2 (from first to third week): normalization of ST changes and flattening of T wave
Stage 3 (from third to fifth week): inversion of T-wave
Stage 4 (from fifth week onwards): gradual normalization of the ECG
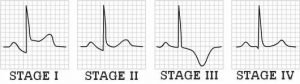
Figure 6: Stages of Acute Pericarditis
Right ventricular pacing effectively treats patients with AV block. This can lead to the phenomena of memory T waves. In patients with intermittent right ventricular pacing abnormal ventricular activation causes inversions of the T-waves after the conversion to sinus rhythm from tachycardia or artificial pacing. The leading theory blames the potassium ion channels for the inappropriate ventricular activation. In such cases, the anterolateral and inferior leads often show deep T-wave inversions (Figure 7). In addition to ventricular pacing, there are other situations in which patients can have memory T-waves such as Wolf-Parkinson-White pre-excitation.
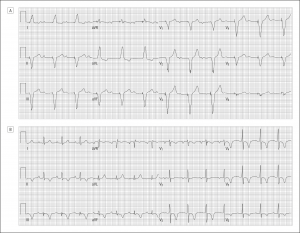
Figure 7: Memory T Waves
Furthermore, electroconvulsive therapy (ECT), an option for treatment-resistant depression, can cause transient T wave inversion. As seen in the EKG below, the precordial leads can show abnormalities (Figure 8) even in patients with no underlying cardiac deficits. The cause has been tied to the increased sympathetic stimulation induced by ECT. A fact further strengthened by the analysis of patients undergoing direct current cardioversion in which T-wave inversions are . However, ECT is not the only treatment that can lead to ECG abnormalities. A dose of >400 mg/day of Flecainide (Tambocor) has been known to cause arrhythmias and T-wave inversions as well. Even illicit drugs, such as cocaine use has been found to cause transient negative T-waves in emergency departments.
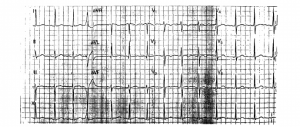
Figure 8: Post ECT
Even an inflammatory disorder, such as sarcoidosis, can lead to T-wave inversions such as those seen below in the inferior leads (Figure 9). Sarcoidosis is a systemic inflammatory condition that manifests with non-caseating granulomas in multiple organs. Involvement with the heart is aptly termed, cardiac sarcoidosis, and it can even mimic another cause of T-wave inversions that will be discussed later, arrhythmogenic cardiomyopathy.
Figure 9: Cardiac Sarcoidosis
The next three pathologies are present in cardiomyopathies and share the common ECG finding of T-wave inversions. However all three can cause a range of symptoms from an absence of symptoms to sudden cardiac death. The first is Brugada syndrome which causes a right bundle branch block in a structurally sound heart due to a mutated sodium channel. Both right and left bundle branch blocks can produce T-wave inversions although uncomplicated blocks more often lack ECG abnormalities. Right blocks (Figure 10) are more likely to produce inversions in leads V1-3 while left blocks more commonly cause inversions in lateral leads such as I, aVL, and V5-6. Bundle branch blocks are associated with ventricular hypertrophy. This aberration of ventricular myocytes would naturally interfere with their repolarization which manifests as T-wave inversions.
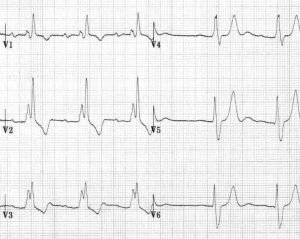
Figure 10: Right Bundle Branch Block
Secondly, Takotsubo cardiomyopathy is a transient form of cardiomyopathy that involves abnormal ballooning of the ventricles in patients that have undergone severe physical or psychological stress. The underlying mechanism relates to the catecholamine excess and the disorder it causes in coronary microvasculature. In the image below (Figure 11), take a look at the precordial leads, V2-6 to see the classic negative T-waves. Additionally, pheochromocytomas share a pathological cause with Takotsubo cardiomyopathy in that both lead to states of catecholamine surplus. Thus the characteristic ECG finding of inversions is also shared by these two pathologies.
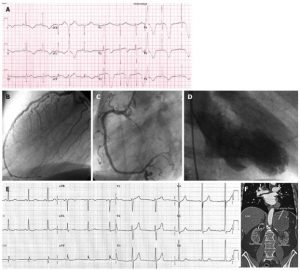
Figure 11: Takotsubo Cardiomyopathy
The third cardiomyopathy that is relevant to the discussion of T-wave inversion is arrhythmogenic cardiomyopathy. A leading cause of sudden cardiac death in patients <35 YO, arrhythmogenic cardiomyopathy (AC) is a disorder that occurs due to the mutation of the plakophilin-2 gene with incomplete penetrance. All the causes of inversion listed above are transient, meaning they exist in a snapshot of time and can be expected to disappear from the patient’s ECG, one way or another. However, arrhythmogenic cardiomyopathy and Yamaguchi syndrome, which will be discussed later, feature permanent T-wave inversions.
In the image below, a patient was found to have precordial T wave inversions with an associated sign of AC, the epsilon wave, which occurs due to postexcitation of right ventricle myocytes (Figure 12).
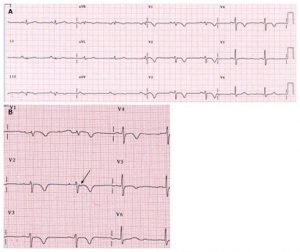
Figure 12: Arrhythmogenic Cardiomyopathy
Next, Yamaguchi syndrome is another condition characterized by permanent T-wave inversions that is more common in the Japanese population. It has a prevalence of 1/2000 to 1/5000 but accounts for 11% of sudden cardiac death in young adults. A form of hypertrophic cardiomyopathy, Yamaguchi syndrome, features an abnormally stiff left ventricle during diastole, which impairs ventricular filling. This pathogenesis more commonly affects the apex of the heart, and thus it is also known as apical hypertrophic cardiomyopathy. Note the T wave inversions and high QRS voltages in the precordial and lateral leads in the image below (Figure 13).
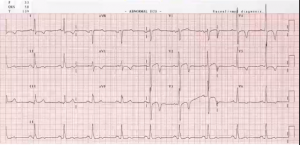
Figure 13: Yamaguchi Syndrome
To summarize, there are a variety of reasons and patterns in the study of T-wave inversions. T-wave inversions can be differentiated by physiologic or pathologic etiology, transient or permanent pattern, cardiac or non-cardiac causes, and the depth, symmetry, or location of the inversions themselves. The next time you see an ECG, keep some of these causes in mind.
Citations
Said, Salah Am. “Cardiac and Non-Cardiac Causes of T-Wave Inversion in the Precordial Leads in Adult Subjects: A Dutch Case Series and Review of the Literature.” World Journal of Cardiology, vol. 7, no. 2, 26 Feb. 2015, p. 86., doi:10.4330/wjc.v7.i2.86.
Burns, ED. “T Wave • LITFL Medical Blog • ECG Library Basics.” Life in the Fast Lane • LITFL • Medical Blog, LITFL, 11 Apr. 2020, litfl.com/t-wave-ecg-library/.
Burns, Ed. “Pericarditis ECG Changes • LITFL • ECG Library Diagnosis.” Life in the Fast Lane • LITFL • Medical Blog, LITFL, 16 Mar. 2019, litfl.com/pericarditis-ecg-library/.
Caforio, Alida. Coronavirus Disease 2019: Myocardial Injury. UpToDate, 2020.
Fagard, R. “Athlete’s Heart.” Heart, vol. 89, no. 12, 2003, pp. 1455–1461., doi:10.1136/heart.89.12.1455.
Littmann, Laszlo. “Large T-Wave Inversion in a Patient With a Pacemaker.” Archives of Internal Medicine, vol. 171, no. 15, 2011, p. 1314., doi:10.1001/archinternmed.2011.358.
Goldberger, Ary. Differential Diagnosis of Basic Electrocardiographic Abnormalities . UpToDate, 2020.
Cockey, George & Conti, C.. (1995). Electroconvulsive therapy-induced transient T-wave inversions on ECG. Clinical cardiology. 18. 418-20. 10.1002/clc.4960180711.
Said, S.a.m., et al. “Flecainide-Induced JT Prolongation, T Wave Inversion and Ventricular Tachycardia during Treatment for Symptomatic Atrial Fibrillation.” International Journal of Cardiology, vol. 44, no. 3, May 1994, pp. 285–287., doi:10.1016/0167-5273(94)90293-3.
Candelario, Nellowe, et al. “Yamaguchi Syndrome Presenting as Atrioventricular Nodal Re-Entrant Tachycardia in an African-American Patient.” BMJ Case Reports, 2017, doi:10.1136/bcr-2016-218051.
McKenna, William. Arrhythmogenic Right Ventricular Cardiomyopathy: Diagnostic Evaluation and Diagnosis. UpToDate, 2019.
