Alyka Glor Fernandez, OMS-IV
Mitchell Dean Maulfair, DO
A previously healthy 16-year-old male presented to the emergency department with abdominal pain, nausea, and vomiting. He woke up with abdominal pain that steadily worsened and was unrelieved by a dose of over the counter simethicone. This prompted his mother to take him to the Emergency Department (ED) for evaluation. In the ED, he complained of dull, achy, non-radiating left lower quadrant abdominal pain. He had a few episodes of emesis that were non-bilious and non-bloody. He denied any other symptoms, including fevers, chills, dysuria, or hematuria.
On physical exam, he was a well-appearing athletic teenager. He was afebrile with stable vital signs. His cardiac exam showed a regular rate and rhythm, and his lungs were clear to auscultation bilaterally. His abdomen was soft, not distended, and completely nontender to palpation in all four quadrants. The genital exam revealed normal male anatomy without testicular tenderness or mass.
The initial workup comprised of basic labs: a complete blood count (CBC), comprehensive metabolic panel (CMP), and urine studies. A creatinine kinase (CK) total was added on to rule out rhabdomyolysis when the initial urine specimen appeared dark in color. A CT scan of the abdomen/pelvis with contrast was obtained.
His CBC and CMP were unremarkable. CK total was within normal limits. However, his urinalysis showed 3+ blood and >50 RBCs. The initial review of the CT scan revealed a normal appendix and no evidence of a mass, adenopathy, nor inflammatory process. His kidneys showed no masses, hydroureter or hydronephrosis. There was no bowel wall thickening, obstruction, mesenteric stranding, or free fluid. On closer inspection, a calcification was noted in the penile urethra, as demonstrated in Figure 1.
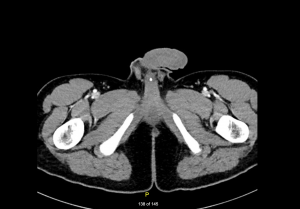
Figure 1. Calcification present in the penile urethra on CT scan.
On reassessment of the patient, he appeared more comfortable but had the urge to urinate. He was given a urine strainer and a 5mm urinary tract stone was collected, as depicted in Figure 2.

Figure 2. A 5mm urinary tract stone collected in urine strainer.
Pediatric urinary stone disease is uncommon compared to adult disease. The Urologic Diseases in America project found the rate of pediatric urinary stone disease in the United States to be about 59.5 cases per 100,000 person-years. 1 As mentioned in the same article, females are affected more than males, and Caucasians also have increased rates of urolithiasis compared to other races and ethnic groups. Children most commonly present with flank or abdominal pain and gross hematuria.2 However, they may present without the symptoms of renal colic, as was the case with our patient. A retrospective study of 1,440 children with urinary calculi in Pakistan found that 55% had stones in the kidney, 14% were ureteral, and 31% were vesical.3 In all patients, but with children especially, the goal with imaging test selection is to minimize radiation exposure as low as reasonably achievable. The American Urological Association recommends an ultrasound as the initial imaging test of choice to screen pediatric patients with suspected urolithiasis.4 Though computed tomography has significantly more radiation exposure than ultrasonography, ultrasound can fail to detect calculi in up to 41% of children with symptoms.5 Thus, in a patient with a negative or indeterminate ultrasound but with a strong suspicion for urolithiasis, a CT scan should be obtained using the low-dose protocol.4 Finding a stone in the urethra on imaging is not common, thus a thing not looked for is seldom found.
References
- Ward JB, Feinstein L, Pierce C, et al. Pediatric Urinary Stone Disease in the United States: The Urologic Diseases in America Project. Urology 2019; 129:180.
- Gearhart JP, Herzberg GZ, Jeffs RD. Childhood urolithiasis: experiences and advances. Pediatrics. 1991;87(4):445-450.
- Rizvi, S., Naqvi, S., Hussain, Z., Hashmi, A., Hussain, M., Zafar, M., Sultan, S. and Mehdi, H., 2002. Pediatric Urolithiasis: Developing Nation Perspectives. Journal of Urology, 168(4 Part 1), pp.1522-1525.
- American Urological Association. Clinical Effectiveness Protocols for Imaging in the Management of Ureteral Calculous Disease: American Urological Association Technology Assessment, 2012. J Urol; April 2013;189(4):1203-1213; DOI: dx.doi.org/10.1016/j.juro.2012.10.031; [cited 2016 Dec 20]. Available from: jurology.com/article/S0022-5347(12)05259-7/fulltext.
- Palmer, J., Donaher, E., O’Riordan N, M. and Dell, K., 2005. Diagnosis of Pediatric Urolithiasis: Role of Ultrasound and Computerized Tomography. Journal of Urology, 174(4 Part 1), pp.1413-1416.
