Flecainide Induced Atrial Flutter Causing Monomorphic Wide Complex Tachycardia
Authors: Dr. Graham Clifford, DO; Dr. Justin Sauter, DO; and Dr. Ben Arnold, MD
Introduction:
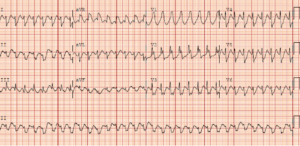
A 65-year-old male with a past medical history of atrial flutter on metoprolol, flecainide and eliquis reported to the Emergency Department for evaluation of palpitations. He related he had undergone transesophageal echocardiographic guided cardioversion in the past for similar symptoms. The patient’s heart rate was noted to be tachycardic at 192 beats per minute. Otherwise, the patient had a normal blood pressure, a normal respiratory rate, normal work of breathing, normal mental status, a cap refill less than 2 seconds in all four extremities and no obvious signs of acute instability. The patient reported uninterrupted anticoagulation. An electrocardiogram (ECG) was performed as shown below.
ECG Iterpretation:
This ECG shows monomorphic wide complex tachycardia (WCT) at a rate of 192 bpm, extreme axis deviation, QRS duration of 160 msec, positive concordance in precordial leads V1-2, negative concordance in precordial leads V3-6 and absence of capture/fusion beats
Clinical Course:
Old electrocardiograms were reviewed and did not reveal any signs of Wolff-Parkinson White syndrome (WPW). This patient’s R-R interval was normal prompting attempts at vagal maneuvers as supraventricular tachycardia (SVT) with aberrancy was on our differential diagnosis list, but we were unsuccessful. Adenosine was administered twice (6mg followed by 12 mg) without success and no notable pauses were observed. The patient was consented for synchronized cardioversion which successfully terminated the arrhythmia with reversion to normal sinus rhythm. Cardiology was consulted early in the patients ED course and reported his WCT likely represented flecainide toxicity causing QRS prolongation and atrial flutter with 1:1 conduction. Cardiology formally interpreted his ECG as “atrial flutter with 1:1 conduction, ventricular rate 192 bpm, with a bundloid QRS morphology”. Cardiology recommended discharge home with instructions to stop flecainide and to increase his metoprolol dose with outpatient clinic follow-up.
Teaching points about wide complex tachycardia (WCT):
- When treating a patient with wide complex tachycardia it is important to treat circulation, airway and breathing in accordance with standard ACLS guidelines. If a patient who is experiencing WCT is deemed unstable, then they should undergo synchronized cardioversion. If a patient who is experiencing WCT is pulseless, then they should undergo cardiopulmonary resuscitation and defibrillation as soon as possible.
- There is observational research to support the use of adenosine in the treatment of stable monomorphic regular WCT. (3)
- There are case reports and studies that describe stable WCT deteriorating to ventricular fibrillation after adenosine administration. (7)
- Adenosine should never be administered without cardiology consultation to a patient with polymorphic WCT, or if an irregular R-R interval is noted, as the patient may have WPW syndrome which places them at risk for degeneration to ventricular fibrillation if given atrioventricular (AV) nodal blocking agents.
- Vagal maneuvers and adenosine can be diagnostic and therapeutic when given in the setting of stable monomorphic wide complex tachycardia. Specifically, there is a therapeutic benefit if the rhythm is SVT with aberrancy as adenosine may terminate the arrhythmia.
- If the patient is suffering from another type of SVT and the QRS complex is wide due to reasons other than ventricular tachycardia you may be able to evaluate P wave morphology after adenosine administration to better attain a diagnosis (e.g., junctional tachycardia, ectopic atrial tachycardia, atrial flutter). This could then alter your treatment modality to the best suited method.
- Lastly, if there is no response to the above-mentioned interventions one can hypothesize that the arrhythmia is generated from the ventricles and ventricular tachycardia is the rhythm at hand. One study showed the odds of ventricular tachycardia increased nine-fold when there was no response to adenosine in the treatment of WCT with adenosine. (5)
Teaching points about flecainide:
- Flecainide is a class IC antiarrhythmic which acts by blocking the sodium channels responsible for phase 0 depolarization of the cardiac action potential.
- Flecainide is typically used to treat atrial fibrillation.
- Flecainide can also cause ventricular and supraventricular arrhythmias.
- Flecainide is known to convert atrial fibrillation into 1:1 atrial flutter where ventricular rates will exceed 200 bpm. The described rate of arrhythmia after flecainide use is 3.5-5%. It is thought to be closely associated with hyperadrenergic states and typically patients taking flecainide are prescribed an AV nodal blocker to avoid this complication. (2)
- The incidence of ventricular dysrhythmias after flecainide administration for conversion of atrial fibrillation has been shown to be less than 3%. (6)
- Flecainide has a small therapeutic window which predisposes the patient to treatment failure and severe adverse reactions when taking it. (1)
- Overdosing of flecainide causes excessive sodium channel blockade manifesting as prolonged PR, QRS, and QT intervals on ECG.
- Flecainide toxicity can cause cardiac arrest not responsive to typical ACLS treatment protocols and may ultimately be responsive to sodium bicarbonate, lipid emulsion therapy and ECMO. (4)
- Flecainide has an FDA black box warning recommending restriction of its use to life-threatening ventricular arrhythmias
Works Cited/Resources:
- Devin R, Garrett P, Anstey C. Managing cardiovascular collapse in severe flecainide overdose without recourse to extracorporeal therapy. Emerg Med Australas. 2007 Apr;19(2):155-9. doi: 10.1111/j.1742-6723.2006.00909.x. PMID: 17448102.
- Falk RH. Proarrhythmia in patients treated for atrial fibrillation or flutter. Ann Intern Med. 1992 Jul 15;117(2):141-50. doi: 10.7326/0003-4819-117-2-141. Erratum in: Ann Intern Med 1992 Sep 1;117(5):446. PMID: 1605429.
- Innes JA. Review article: Adenosine use in the emergency department. Emerg Med Australas. 2008 Jun;20(3):209-15. doi: 10.1111/j.1742-6723.2008.01100.x. PMID: 18549383.
- Khatiwada P, Clark L, Khunger A, Rijal BB, Ritter J. A Case Report of Flecainide Toxicity With Review of Literature. Cureus. 2022 Feb 15;14(2):e22261. doi: 10.7759/cureus.22261. PMID: 35350525; PMCID: PMC8933271.
- Marill KA, Wolfram S, Desouza IS, Nishijima DK, Kay D, Setnik GS, Stair TO, Ellinor PT. Adenosine for wide-complex tachycardia: efficacy and safety. Crit Care Med. 2009 Sep;37(9):2512-8. doi: 10.1097/CCM.0b013e3181a93661. PMID: 19623049.
- McNamara RL, Tamariz LJ, Segal JB, Bass EB. Management of atrial fibrillation: review of the evidence for the role of pharmacologic therapy, electrical cardioversion, and echocardiography. Ann Intern Med. 2003 Dec 16;139(12):1018-33. doi: 10.7326/0003-4819-139-12-200312160-00012. PMID: 14678922.
- Parham WA, Mehdirad AA, Biermann KM, Fredman CS. Case report: adenosine induced ventricular fibrillation in a patient with stable ventricular tachycardia. J Interv Card Electrophysiol. 2001 Mar;5(1):71-4. doi: 10.1023/a:1009810025584. PMID: 11248777.
