Dhimitri A Nikolla, DO, PGY-4
LECOM-Erie
CASE
An elderly male with a past medical history of dementia, on warfarin for a remote history of pulmonary embolism, presented via ambulance from a skilled nursing facility due to the facility’s reports of altered mental status and decreased oral intake. On the day of presentation, he had completed a course of amoxicillin/clavulanate for aspiration pneumonia and was given a dose of ceftriaxone for a suspected urinary tract infection diagnosed the same day. His vital signs included a temperature of 32.9 degrees C, heart rate of 68 beats per minute, respiratory rate of 41 breaths per minute, blood pressure of 116/74 mmHg, SpO2 96% RA. He was agitated, tugging his Foley catheter with a normal cardiopulmonary and abdominal examinations. His chest radiograph revealed left basilar infiltrates (Figure 1) and he had an elevated lactic acid at 3.1 mmol/L. Troponin and calcium levels were normal. An electrocardiogram (ECG) was obtained and compared to his prior ECG (Figures 2 and 3).

Figure 1 displays the chest radiograph of the patient.

Figure 2 displays the electrocardiogram of the patient at presentation.
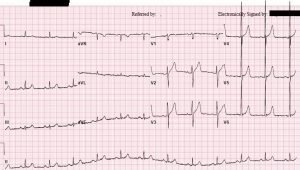
Figure 3 displays the prior electrocardiogram of the patient.
What classic finding can be seen on the electrocardiogram and what is the etiology?
DISCUSSION
Osborn or J waves due to hypothermia. The phenomenon is named after John Osborn who described the finding in 1953 on ECGs of canines with induced hypothermia, though descriptions of the wave were reported earlier in the literature [1-2]. This unique deflection of the J point is most commonly caused by hypothermia, but has many other etiologies (Figure 4). It can also be mistaken for the J point elevation seen in Brugada syndrome; however, Osborn or J waves usually present in the inferior or lateral leads, while Brugada J point elevation usually presents in the right precordial leads (Figure 5) [1,3]. The arrhythmogenicity of Osborn or J waves is unclear, but the underlying causes, such as critical hypothermia, are likely the culprit [1,5,6].
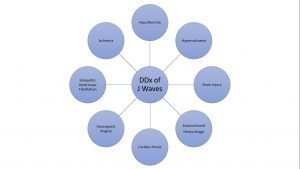
Figure 4 displays the differential diagnosis of Osborn or J waves.
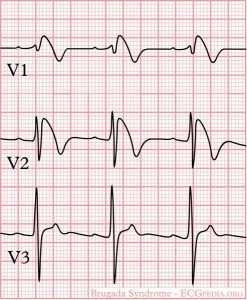
Figure 5 displays the typical J point elevation with a coved-type ST segment elevation seen in Brugada syndrome [3,4].
CONCLUSION
The patient was admitted to the intensive care unit on vancomycin, cefepime, and azithromycin. The lactic acidosis resolved and his mental status improved. He was discharged on hospital day 4 back to his nursing home.
REFERENCES
- Maruyama M, Kobayashi Y, Kodani E, et al. Osborn Waves: History and Significance. Indian Pacing Electrophysiol J. 2004;4(1):33–39.
- Osborn JJ. Experimental hypothermia: Respiratory and blood pH changes in relation to cardiac function. Am J Physiol 1953;175:389-398.
- Brugada J, Campuzano O, Arbelo E, Sarquella-Brugada G, Brugada R. Present Status of Brugada Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018 Aug 28;72(9):1046-1059.
- CardioNetworks: Googletrans (5/10/12, 17:19). De-Brugada. Wikimedia Commons. Creative Commons Attribution-Share Alike 3.0 Unported license. Accessed: 1/31/19. < https://commons.wikimedia.org/wiki/File:De-Brugada_(CardioNetworks_ECGpedia).png>
- Zafren K, Mechem CC. “Accidental hypothermia in adults.” UpToDate. Accessed: 11/27/18. <https://www.uptodate.com/contents/accidental-hypothermia-in-adults#H1>
- Nikolla DA. A Case and Discussion of Accidental Hypothermia in the Setting of Trauma. The Fast Track. Winter 2019. Published Online: 1/15/18. <https://acoep-rso.org/the-fast-track/a-case-and-discussion-of-accidental-hypothermia-in-the-setting-of-trauma/>
