Dhimitri Nikolla, DO, PGY-4
AHN Saint Vincent Hospital
Erie, PA
CASE
A 22-year-old male presented as a trauma alert completely unresponsive. He was found down by a bystander, unresponsive with significant facial trauma presumed to be from assault. Upon arrival, the patient had apneic respirations being assisted by emergency medical service personnel with bag-valve-mask ventilations. He had bilateral breath sounds, a weak, bradycardic pulse, and was unresponsive with a Glasgow Coma Scale of 3. The patient was intubated with rapid sequence intubation and a left femoral vein introducer was placed emergently due to inadequate peripheral access. His initial vital signs were BP 90/palp, HR 43 BPM, SpO2 99%, and temperature 27 ⁰C. The secondary survey revealed multiple facial contusions and a large laceration to the left chin. His electrocardiogram is displayed in Figure 1.
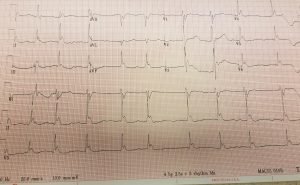
Figure 1 displays the patient’s electrocardiogram revealing atrial fibrillation with a junctional escape rhythm and Osborn or J waves.
DISCUSSION
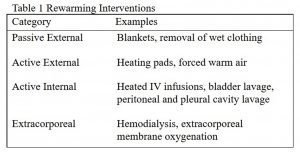
Accidental hypothermia is common among trauma patients, occurring up to 49.6% of cases [1]. Although the etiology of hypothermia can vary, the most common mechanisms include convective and conductive heat loss from exposure to cold air and water [2]. While several systems exist to stage hypothermia, the “Swiss System” is commonly used (Figure 2) [2-4]. Patients in higher stages of hypothermia often require more invasive rewarming interventions, but it is best to take a stepwise approach from least invasive to more invasive (Table 1) [2].
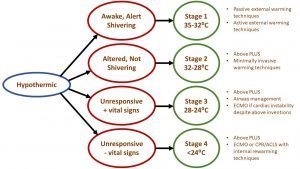
Figure 2 displays a variation of the Swiss System of staging hypothermia with levels of interventions that may be required at each stage [2-4].
Cardiac irritability in the setting of hypothermia can cause various types of dysrhythmias and electrocardiographic abnormalities. Severe bradycardia can occur, though cardiac pacing is usually not needed. However, if pacing is needed, transcutaneous pacing is preferred over transvenous due the risk of the wire touching the irritable heart and inducing a ventricular dysrhythmia [2,6]. Atrial fibrillation and atrial flutter can also occur, but usually resolve with rewarming. When ventricular dysrhythmias and asystole occur in the setting of hypothermia, advanced cardiac life support interventions such as defibrillation and vasopressors may be ineffective until rewarming has occurred. Other electrocardiographic changes include J point elevation, otherwise known as Osborn or J waves. Usually seen in the precordial leads, the height of the J wave is related to the severity of hypothermia [2].
Accidental hypothermia in the setting of trauma raises particular concern compared to the atraumatic hypothermic patient. From a physiological standpoint, coagulopathy can by exacerbated and the inflammatory response suppressed, making bleeding and infection a greater concern [2,5]. If central venous access is needed, femoral lines are preferred as internal jugular and subclavian lines that physically touch the irritable, hypothermic heart may cause ventricular dysrhythmias. Left sided chest tubes carry a similar risk of dysrhythmias. Lastly, while hypothermia causes peripheral vasoconstriction to retain heat, peripheral vasodilation can occur during rewarming causing a phenomenon known as core temperature afterdrop. Core temperature afterdrop causes a decrease core temperature after initiation of rewarming, which is associated with hypotension and acidemia [2]. These physiological changes may create diagnostic uncertainty in a previously stable trauma patient and may worsen hemodynamics in an already unstable trauma patient. Core temperature after drop may be mitigated by rewarming the core first, then the extremities (ie. placing a warming blanket over the core while leaving the extremities exposed) [2].
CASE CONCLUSION
Computed tomography scans revealed a small traumatic subarachnoid hemorrhage and multiple facial fractures including an open fracture to the left mandible. Laboratory studies revealed a lactic acid of 6.3 and a potassium level of 2.9. His hypothermia resolved within about 3 hours with a combination of warm saline infusion, a forced air warming blanket, and warm saline bladder lavages every ten minutes. The following day, the patient went to the operating room for debridement and open reduction internal fixation of his open mandible fracture. Two days after presentation he was extubated with no neurological deficits.
REFERENCES
- Helm, et al. Accidental hypothermia in trauma patients. Is it relevant to preclinical emergency treatment? Anaesthesist. 1995;44(2):101-7.
- Zafren K and Mechem CC. “Accidental hypothermia in adults.” UpToDate. https://www.uptodate.com/contents/accidental-hypothermia-in-adults#H1. Accessed: 11/27/18.
- Durrer B, Brugger H, Syme D. The Medical On-site Treatment of Hypothermia: ICAR-MEDCOM Recommendation. High Alt Med Biol. 2003;4(1):99-104.
- Brown DJA, Brugger H, Boyd J, Paal P. Accidental Hypothermia. N Engl J Med. 2012;367(20):1930-1938.
- Vardon F, et al. Accidental hypothermia in severe trauma. Anaesth Crit Care Pain Med. 2016;35(5):355-361.
- Ho JD, Heegaard WG, Brunette DD. Successful transcutaneous pacing in 2 severely hypothermic patients. Ann Emerg Med. 2007;49(5):678.
