Dhimitri Nikolla, DO, PGY-4
AHN Saint Vincent Hospital
Erie, PA
Case
A 70-year-old female with a past medical history of severe COPD presents complaining of dyspnea and right-sided chest pain for 4 days. Triage vital signs include a blood pressure of 201/95 mmHg, heart rate of 87 beats/minute, temperature 36.4 degrees Celsius, respiratory rate of 24 breaths/minute, and oxygen saturation of 97%. Physical examination reveals regular heart beats without murmur. Decreased breath sounds on the right. Strong radial pulse is present. A chest radiograph is obtained (Figure 1).

Figure 1. Initial PA chest radiograph.
Diagnosis
Spontaneous Tension Pneumothorax. Pneumothorax occurs when air gets trapped in the pleural space, the space between the lung and chest wall. There are various types and etiologies (Figure 2), but a tension pneumothorax occurs when the intrathoracic pressure rises more than 15-20 mmHg compressing the heart and mediastinum restricting cardiac preload and thereby reducing cardiac output.
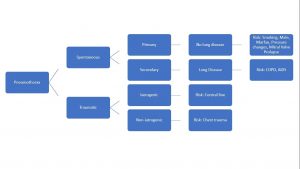
Figure 2. Categorization of pneumothorax etiology and risk factors.
This classically causes shifting of the trachea and mediastinum to the contralateral side on chest radiography, but chest radiography can miss up to 17% in the upright and 80% in the supine positions. Ultrasound evaluation for lung sliding is more sensitive than chest radiography, but computed tomography is most sensitive often finding occult pneumothoraces that require no intervention.
Several ways exist to estimate the size of a pneumothorax, but a 2 cm interpleural distance at the level of the hilum roughly correlates with a size of 50% lung volume. A small vs a large pneumothorax can be determined by an interpleural distance of < or > 2 cm. Figure 3 displays another large tension pneumothorax occurring after chest compressions post cardiac arrest.

Figure 3. A large tension pneumothorax on AP chest radiograph with an interpleural distance of 2.58cm.
While clinically stable, small pneumothoraces <20% lung volume may be treated with oxygen and observation, immediate needle decompression followed by chest tube placement should be performed for tension pneumothorax with clinical instability. Small-bore catheters are a viable option but may not be able to handle the air flow from a large air leak; therefore, a larger chest tube may be needed.
Case Conclusion
The patient is clinically stable; therefore, an 8 French pig-tail catheter is placed primarily with successful re-expansion of the lung seen on repeat chest radiograph (Figure 4). The patient has an uncomplicated hospital course without recurrence of her pneumothorax. The pig-tail catheter is removed on hospital day 3 and she is discharged.
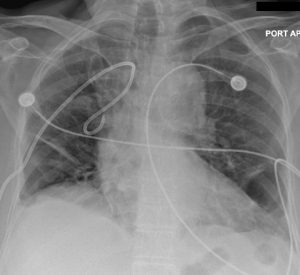
Figure 4. Repeat AP chest radiograph after placement of an 8 French pig-tail catheter with resolution of the tension pneumothorax.
References
Tintinalli JE, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016. Chapters 68 & 261.
