Taylor A. Klein, MS, OMS-IV
Nicholas S. Bowman, OMS-IV
If conversations in your household are anything like ours, we are rapidly approaching our regularly scheduled influenza debate. The arguments are numerous:
“That vaccine never works anyway.”
“Any time I get that vaccine, I get the flu from it.”
“I’ve been fine without it this long. I’m not starting now.”
“Isn’t there mercury in that?”
And around… And around… No matter how many degrees we wear behind our names or what accolades we carry, the debate goes on. Sometimes it feels easier to take the loss than to exhaust ourselves on a futile endeavor. And so, in a world where most of the debate is centered around controlling the spread of COVID-19, mask mandates, and a potential future COVID vaccine, it may feel easier to let old demons lie. However, this year, it has become more important than ever to win the influenza debate.
In an average year, influenza season lasts between 11 and 20 weeks during the fall and into the winter. In 2018-2019, the flu season lasted a total of 21 weeks, the longest flu season in a decade (Nessel, 2019), and sickened an estimated 35,520,883 people (Past Seasons Estimated Influenza Disease Burden | CDC, n.d.). Figure 1 shows the most common flu months. More than 490,000 of these patients were hospitalized and more than 34,000 ultimately succumbed to their illness (<1% mortality rate). Approximately 30-40% of laboratory-confirmed influenza patients hospitalized in any given year are diagnosed with acute pneumonia and are at higher predisposition for bacterial sepsis and ARDS (Kalil & Thomas, 2019). Perhaps, most tragically, approximately 80% of reported pediatric deaths occurred in unvaccinated children.
Over the past 9 months, we’ve had a new viral respiratory illness take center stage and present new concerns. Figures 2 and 3 show the current statistics regarding COVID-19 cases. Early reports out of China estimated the inpatient mortality of SARS-CoV-2 quite high at approximately 28% (Weiss & Murdoch, 2020). This risk significantly increased with older patient age, increased Sequential Organ Failure Assessment (SOFA) score, elevated d-dimer, and presence of other comorbidities including hypertension and coronary artery disease (Zhou et al., 2020).
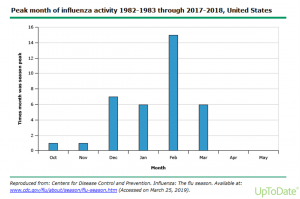
Figure 1. Most common flu season time frames (The Flu Season | CDC, n.d.)
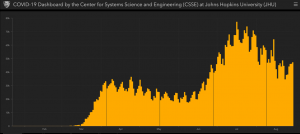
Figure 2. Daily reported coronavirus cases in the US as of 08/30/2020
(COVID-19 Map – Johns Hopkins Coronavirus Resource Center, n.d.)
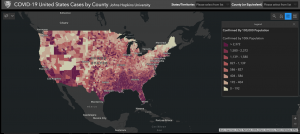
Figure 3. Confirmed cases of coronavirus on the mainland United States as of 08/30/2020
(COVID-19 United States Cases by County – Johns Hopkins Coronavirus Resource Center, n.d.)
Unfortunately, ongoing research has suggested that it is possible for a single patient to be coinfected with both COVID-19, influenza, and other viral respiratory infections. The statistics are still developing but rates of coinfection have been reported from 3.2 – 20.7% (X. Chen et al., 2020). Coinfected patients require higher levels of care, have increased length of stays, and significantly increased risk of Acute Respiratory Distress Syndrome (ARDS) due to both viruses increasing cytokines and inflammatory cells in the lungs. ARDS may lead directly to respiratory failure, the leading cause of death in fatal COVID-19 cases (Tay et al, 2020).
In addition to the methods put in place to mitigate viral spread in response to COVID including social distancing, mask mandates, and a transition to more virtual interactions, the best way to mitigate coinfection with influenza is the same as it has been every year. It is important to receive the annual influenza vaccine. Last year, research was completed to estimate the efficacy of the influenza vaccine for 2019-2020 (Dawood et al., 2020). Of the 4,112 patients in this study with an acute respiratory illness, 1,060 tested positive for influenza. This population had between 40-60% vaccination rates. This means that with 100% vaccine compliance, infection rates could be cut in half or doubled without the vaccine. COVID-19’s transmissibility is almost double that of influenza, suggesting the number of coinfections will rapidly increase as flu season accelerates (T. Chen et al., 2016; Sanche et al., 2020).
Additionally, early avenues of research have suggested that a potential protective effect may exist of the influenza vaccine on COVID-19 mortality – even without influenza coinfection, specifically in elderly, vulnerable populations (Zanettini et al., 2020). This is hypothesized to be due to vaccinated individuals having lower rates of respiratory complications due to influenza, leaving a more robust reserve to respond to COVID infection.
The evidence is clear. The vaccine works. The vaccine does not give you the flu. You may have been fine without it, but the individuals you give it to may not be. It does not contain mercury. What the vaccine does is save lives and keeps our population heathy. COVID-19 is overwhelming and there is a lot of misinformation publicized. But what is true is this: if you get your flu vaccine, you will save someone’s life.
REFERENCES
Chen, T., Chen, T., Liu, R., Xu, C., Wang, D., Chen, F., Zhu, W., Zhang, X., Yang, J., Wang, L., Xie, Z., Chen, Y., Bai, T., Li, Y., Wang, Z., Zhang, M., Chen, S., & Shu, Y. (2016). Transmissibility of the Influenza Virus during Influenza Outbreaks and Related Asymptomatic Infection in Mainland China, 2005-2013. PLOS ONE, 11(11), e0166180. https://doi.org/10.1371/journal.pone.0166180
Chen, X., Liao, B., Cheng, L., Peng, X., Xu, X., Li, Y., Hu, T., Li, J., Zhou, X., & Ren, B. (2020). The microbial coinfection in COVID-19. Applied Microbiology and Biotechnology, 1. https://doi.org/10.1007/s00253-020-10814-6
COVID-19 Map – Johns Hopkins Coronavirus Resource Center. (n.d.). Retrieved August 30, 2020, from https://coronavirus.jhu.edu/map.html
COVID-19 United States Cases by County – Johns Hopkins Coronavirus Resource Center. (n.d.). Retrieved August 30, 2020, from https://coronavirus.jhu.edu/us-map
Dawood, F. S., Chung, J. R., Kim, S. S., Zimmerman, R. K., Nowalk, M. P., Jackson, M. L., Jackson, L. A., Monto, A. S., Martin, E. T., Belongia, E. A., McLean, H. Q., Gaglani, M., Dunnigan, K., Foust, A., Sessions, W., DaSilva, J., Le, S., Stark, T., Kondor, R. J., … Flannery, B. (2020). Interim Estimates of 2019–20 Seasonal Influenza Vaccine Effectiveness — United States, February 2020. MMWR. Morbidity and Mortality Weekly Report, 69(7), 177–182. https://doi.org/10.15585/mmwr.mm6907a1
Kalil, A. C., & Thomas, P. G. (2019). Influenza virus-related critical illness: Pathophysiology and epidemiology. In Critical Care (Vol. 23, Issue 1). BioMed Central Ltd. https://doi.org/10.1186/s13054-019-2539-x
Nessel, J. (2019). CDC: 2018-2019 Flu Season the Longest in a Decade. Pharmacy TImes. https://www.pharmacytimes.com/resource-centers/flu/cdc-20182019-flu-season-the-longest-in-a-decade
Past Seasons Estimated Influenza Disease Burden | CDC. (n.d.). Retrieved August 25, 2020, from https://www.cdc.gov/flu/about/burden/past-seasons.html
Sanche, S., Lin, Y. T., Xu, C., Romero-Severson, E., Hengartner, N., & Ke, R. (2020). High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerging Infectious Diseases, 26(7), 1470–1477. https://doi.org/10.3201/eid2607.200282
The Flu Season | CDC. (n.d.). Retrieved August 30, 2020, from https://www.cdc.gov/flu/about/season/flu-season.htm
Weiss, P., & Murdoch, D. R. (2020). Clinical course and mortality risk of severe COVID-19. In The Lancet (Vol. 395, Issue 10229, pp. 1014–1015). Lancet Publishing Group. https://doi.org/10.1016/S0140-6736(20)30633-4
Zanettini, C., Omar, M., Dinalankara, W., Imada, E. L., Colantuoni, E., Parmigiani, G., & Marchionni, L. (2020). Influenza Vaccination and COVID19 Mortality in the USA. MedRxiv, 2020.06.24.20129817. https://doi.org/10.1101/2020.06.24.20129817
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., Xiang, J., Wang, Y., Song, B., Gu, X., Guan, L., Wei, Y., Li, H., Wu, X., Xu, J., Tu, S., Zhang, Y., Chen, H., & Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet, 395(10229), 1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3
