Christopher Hart, OMS-II @LECOM-Erie
Dhimitri A Nikolla, DO, PGY-4 @AHN Saint Vincent Hospital
INTRODUCTION
Emergency physicians often have difficulty dispositioning patients presenting to the emergency department (ED) with acute dyspnea caused by exacerbations in either chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF). This may be due to a lack of clear and consistent guidelines, but also likely due to the high frequency of ED and hospital readmissions despite treatment [1-3]. Readmission rates in 30 days can be as high as 10-20% in COPD and 35.5% in CHF, and predicting those who return can be challenging [4-5]. While much data exists on the use of various walk tests to prognosticate COPD and CHF outpatients [6-7], limited data exists on the ED walk test for patients in COPD and CHF exacerbation to aid in disposition decisions.
THE EVIDENCE
Although different variations of the walk test exist, the best evidence is likely for the 3-minute ED walk test (3MWT). The primary purpose of the 3MWT is to determine patients at risk of serious adverse events despite ED treatment. Serious adverse events include death within 30 days of the ED visit, admission to a critical care unit, intubation, noninvasive ventilation, major procedure, or myocardial infarction [2-3].
All Comers
In a prospective cohort study of 40 adult ED patients with COPD, CHF, or stable chest pain, 30% of patients had a poor outcome. 41.7% of those with a poor outcome could not complete the 3MWT compared with 3.6% of those with a good outcome [1].
CHF Exacerbation
Failure of the 3MWT, including being too ill to partake, tachycardia ≥110bpm, and hypoxemia SpO2<90% during the test, has been associated with serious adverse events in CHF exacerbations [3,8]. A study of 559 patients with heart failure showed that among the 65 patients who experienced serious adverse events, 32.3% of them failed the 3MWT. Only 10.7% of the 494 patients who did not experience adverse events failed [3]. A prospective cohort study of 1,100 CHF patients across 6 EDs revealed that of the 170 patients who experienced serious adverse events, 70.3% failed the 3MWT compared to 53.1% of those without serious adverse events [8].
COPD Exacerbation
Failure of the 3MWT, including being too ill to partake, tachycardia ≥120bpm, and hypoxemia SpO2<90% during the test, has been associated with serious adverse events in COPD exacerbations [2]. In a study of 945 COPD patients, 74 had serious adverse events and 41.9% of those failed the 3MWT compared to only 13% of those without serious adverse events [2].
HOW IS IT DONE
The 3MWT is performed after ED treatment and prior to discharge. Baseline heart rate and SpO2 are obtained prior to test. The patient is instructed to walk at their own pace in the ED for three minutes, covering any distance they can within the time-frame. Assistance with walking aids is permitted; however, the patient may not be assisted by any person. Additionally, no supplemental oxygen is given to the patient apart from their baseline home oxygen supplementation. During the walk, the highest heart rate and lowest SpO2 are documented. After walking for three minutes, the heart rate and SpO2 are measured one minute after completion (Figure 1) [3]. The patient fails the 3MWT with any of the previously described criteria (Figure 2).

Figure 1 displays the steps to the 3MWT.
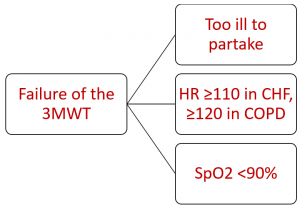
Figure 2 displays the ways patients can fail the 3MWT.
CONCLUSION
While the 3MWT should not be used in isolation, failure of the 3MWT by CHF and COPD exacerbation patients in the emergency department may help the clinician better predict their risk of serious adverse events and assist with disposition.
REFERENCES
- Pan AM, Stiell IG, Clement CM, Acheson J, Aaron SD. Feasibility of a structured 3-minute walk test as a clinical decision tool for patients presenting to the emergency department with acute dyspnoea. Emerg Med J. 2009 Apr;26(4):278-82.
- Stiell IG, Clement CM, Aaron SD, et al. Clinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort study. CMAJ. 2014 Apr 1;186(6):E193-204.
- Stiell IG, Clement CM, Brison RJ, et al. A risk scoring system to identify emergency department patients with heart failure at high risk for serious adverse events. Acad Emerg Med. 2013 Jan;20(1):17-26.
- Simmering JE, Polgreen LA, Comellas AP, Cavanaugh JE, Polgreen PM. Identifying patients with COPD at high risk of readmission. Chronic Obstr Pulm Dis.2016;3(4):729-738.
- Bergethon KE, Ju C, DeVore AD, et al. Trends in 30-Day Readmission Rates for Patients Hospitalized With Heart Failure: Findings From the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail. 2016 Jun;9(6). pii: e002594.
- Zeng GS, Chen LC, Fan HZ, et al. The relationship between steps of 6MWT and COPD severity: a cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2018 Dec 28;14:141-148.
- Ingle L, Cleland JG, Clark AL. The relation between repeated 6-minute walk test performance and outcome in patients with chronic heart failure. Ann Phys Rehabil Med. 2014 Jun;57(4):244-53.
- Stiell IG, Perry JJ, Clement CM, et al. Prospective and Explicit Clinical Validation of the Ottawa Heart Failure Risk Scale, With and Without Use of Quantitative NT-proBNP. Acad Emerg Med. 2017 Mar; 24(3):316-327
