Samuel James Nobilucci, DO, MSM-HCA, EMT-P
Emergency medicine (EM) is a complex and adaptive specialty that blends the knowledge base of a general practitioner with aspects from nearly every other specialty. Be it pediatrics, geriatrics, infectious disease, surgery, or any number of organ-based focuses, there’s no limit to what may come through the doors at any given moment. We as emergency physicians are expected to have the knowledge, skills, and attitudes required to not only respond to these situations with the highest level of care, but to do so effectively while managing every patient in our charge with the same level of responsibility.
The complexity can be daunting for students and new medical school graduates beginning their EM careers as interns. I myself was one of the overwhelmed, and while I had received more than enough preparation through medical school education, I initially lacked both the perspective and the necessary mindset to grasp these principles to the appropriate degree.
I attended medical school at a University that focused on providing a strong foundation in primary care, giving me an excellent education in the principles of general medicine. There we trained in patient communication, education, and continuity of care. I graduated from this institution with the breadth of knowledge characteristic to most freshly minted physicians, but with limited experience in any particular specialty.
When I matched into emergency medicine, I was welcomed quickly by the cold realities of the profession. I could no longer spend extended time with each patient obtaining a history and physical exam. Workups seemed rushed and incomplete, and patients rarely (if ever) appeared to be active partners in their own healthcare team.
My frustration grew as I watched my intern colleagues adapt to this structure and begin to flourish in their new roles. There were concerns stated by attending physicians about my lack of progress within the program. My barriers seemed insurmountable as I told my program director that I believed I had chosen the wrong specialty. To his credit, this physician did not balk at my statement. Rather, he calmly and coolly assured me that while he believed that once I found my footing I would indeed become a great emergency physician, he would support me fully in whatever decision I made. As an aside: this statement is largely the reason I remain in emergency medicine, and I am forever indebted to his kindness and understanding.
With newfound determination to succeed, I turned to my training in business administration to find an answer to my problem. While an early step in my success appeared to be gaining a more thorough understanding of the expectations within my program, the FIRST step required a definition of the overarching framework I was expected to function within.
Emergency medicine is indeed a generalized knowledge base; it may actually be the most diverse medical specialty practiced – yet we are absolutely specialists in our own right! While emergency physicians may see everyone from birth to death with every malady imaginable in between, we approach each patient in a manner unique to our craft. Our specialty is efficiency: efficiency in time, efficiency in testing, efficiency in intervention. Everything comes down to providing the highest level of care in the shortest amount of time before sending the patient to their next stage of evaluation and management.
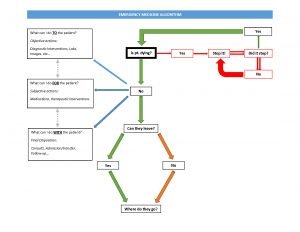
“So what is efficiency in care”, I asked myself. How do I condense the global knowledge of a general practitioner into the highly focused, acute and expedited world of emergency medicine? In true emergency medicine fashion, I designed an algorithm. This drastically turned the tide of my own practice, and I have used it with my own students and interns with great success. In emergency medicine we tell our students that the first step in patient care is to determine a “sick-or-not-sick” snapshot from our initial moments of an encounter. One of my attending physicians stressed this concept by frequently allowing me only a glimpse of the patient, no more than a few seconds, before asking me my general impression.
Of course, this assessment can change at any moment and requires a great deal of foresight and experience to become proficient. It is also not necessarily obvious to determine the patient’s status without a much deeper inspection. While “sick” may be something that we are comfortable assessing based on general appearance, vital signs, etc… “not sick” is a difficult and sometimes dangerous statement as developing illness or injury combined with various compensatory mechanisms may mask a serious underlying issue. For this reason, we start our pathway in the EM Algorithm by asking bluntly (to ourselves) “is the patient [imminently] dying?” If the answer is “yes,” then the ultimate purpose of emergency medicine is realized in life-saving intervention and we proceed on our pathway to the logical next step of, “stop it.” Within this cycle is the perilous process. We may proceed through this step of intervention and reassessment several times before emerging from it with a living, or deceased patient. Needless to say, the more times we continue through this cycle, the less likely it becomes that we escape it. However, if we are able to halt the dying process, then we can change the answer to our initial question by stating “no.”
Once we have established that our patient is not in immediate mortal danger, we must work on determining their disposition. These final destinations (from our framework) are ultimately reached by a process that I have simplified through the three-step model listed as “What can I do TO/FOR/WITH the patient.” While these questions exist far more on a continuum than I am able to portray in this algorithm, they involve performing objective diagnostic tests and interventions TO the patient in order to determine the extent of their illness or injury. We provide therapeutic interventions and medications FOR the patient to ease pain, anxiety, or discomfort, and we finally must decide what to do WITH the patient for their final disposition and follow up. This final step can also have a double meaning. As including the patient in their management plan is important to empowering the patient and ensuring compliance.
Regarding the last step in the algorithm, we must ask ourselves, “can the patient leave [the hospital]?” If “yes”, then we must provide them with the necessary referrals, education and directions for appropriate follow up, as well as any prescriptions for medications or additional testing required. If the answer is “no” and the patient requires hospital admission, we must consult the appropriate admitting service, and often additional specialists required in their ongoing care.
The EM Algorithm reduces the immensity of emergency medicine into a three-step process. Once I was able to grasp this principle my performance and job satisfaction improved significantly. I was able to focus on patient communication and education, on thorough and complete workups, and on developing partnerships with patients in their own health and well-being. Only now I feel I was able to do so with efficiency, confidence, and a sense of purpose.
In the spirit of lifelong learning, I know that this algorithm and my mindset will be adapted continuously over the course of my career, hopefully with the same primary focus on the patient through communication, education, and care. I hope that my experience will lend some benefit to others who may be going through similar obstacles. You can do this! As always, keep up the great work and stay safe out there!
