Authors:
Paige Reinfeld, MS, OMS-II
Shriman Balasubramanian, MS, OMS-II
Michael Polito, OMS-II
Nicole Kiess, OMS-II
Adithya Nagaraja, OMS-II
School: TouroCOM – Middletown,NY
Social Media: @simclubtouro
Introduction
Airway management remains an essential skill for various healthcare disciplines, with the recognition and management of difficult airways being most challenging.1 A significant source of mortality and morbidity stems from provider failure at properly managing airways efficiently.2,3 Simulation training in advanced airway management provides opportunities to reduce medical errors and improve patient safety outcomes significantly. Simulation training provides a realistic environment where healthcare providers can practice and perfect their skills with zero risk of patient harm.2,4 The stress time-pressured situation of an emergency airway simulated scenario can provide this realistic training to strengthen communications skills, crisis management, and technical resource utilization.2,5 Of concern for training facilities which are employing the use of airway simulation devices, is the cost of these training modalities, and making the decisions as to which are the most useful. This paper aims at discussing a specific type of difficult airway management utilizing the Suction-Assisted Laryngoscopy Assisted Decontamination (SALAD) simulation system.1 Emphasis is placed on ways that simulation centers can cost-efficiently and effectively build their own SALAD for training purposes.
Materials/Methods
Table 1. Materials purchased for the SALAD system and their costs
| Component | Price |
| 20 pack of 8 inch Cable Ties | $2.56 |
| 3 of Polypropylene ½ inch pipe thread adapter | $0.99 |
| ½ inch valve adapter washer | $13.76 |
| 2 ½ inch PVC Sch. coupling devices | $1.38 |
| Becket 160 GPH submersible pump | $29.98 |
| 54 gallon plastic bucket | $20 |
| ½ inch twister two sided coupling device | $0.35 |
| 20 foot clear vinyl tubing | $9.21 |
| 2 gallon red cooler | $9.97 |
| Total | $88.20 |
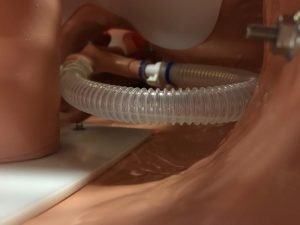
The SALAD simulator at Touro COM was build using readily available and cost-effective materials in order to ensure that it can be replicated in multiple settings. We also used a standard suction setup and an airway trainer torso that was not in use anymore due to an anatomical defect. It was found that this anatomical defect made it a good candidate for this simulator because it qualified as a difficult airway. The goal is to simulate active bleeding or vomiting in the airway during intubation, and most of the items purchased went towards this purpose. The mannequin setup involves first removing any connections that were attached to the esophagus and trachea. Then, PVC tubing suitable for water pressure was attached to the distal end of the mannequin’s esophagus to be connected to the water pump. Additionally, the right and left main-stem bronchi were connected via tubing to each other so that any fluid that mistakenly went into the trachea would be regurgitated back into the pharynx.
The pump is set up to be submerged in liquid at all times, and has multiple settings on it so that the instructor leading the simulation can change the volume and speed of secretions. This pump is to be submerged in water in the 2-gallon cooler, and the spigot of the cooler is connected to PVC tubing that connects to the esophageal tubing end. Now that there is a flow of fluid from the cooler into the esophagus, we wanted to have a way to put fluid back into the cooler. To accomplish this, the mannequin is to be placed in the 54-gallon tote with one side cut out during simulations to allow room for airway personnel. A small hole is cut in the tote near the bottom, and tubing is attached that leads to the top of the cooler. This allows for any secretions not collected by suction to flow back into the cooler to be reused. Multiple tube coupling devices and cable ties are used throughout tubing to ensure a proper seal under higher amounts of pressure. Lastly, the suction setup is a standard portable suction unit with the appropriate tubing and Yankauer suction tip are used. However, this can be easily changed out for French suction for post-intubation management.
Results
The completion of this mannequin results in an innovative, cost-effective way to create a SALAD trainer as shown by pictures in the appendix. The subtotal cost of the materials excluding the airway trainer and suction setup was $88.20, with tax varying by location. We exclude the standard airway trainer and suction setup in our total cost because these were reused from Touro COM’s Simulation Lab. The simplistic approach to this allows for alterations to be made as our demands change, but also for multiple techniques to be used. This SALAD system is compatible with Mac and Miller blades, bougie assisted intubation, as well as alternative devices such as a video laryngoscope. The device was tested in Touro COM’s Simulation Lab during the Osteopathic Medical Student II Medical Simulation class in Fall 2018, and was successful in providing students valuable and realistic experience and feedback on managing a difficult airway using a team-based approach.
Discussion
The medical simulation program at our institution provides a vital first look and practice of clinical skills for medical students. In order to give our students more opportunities to practice skills hands-on without limiting ourselves financially, we have pursued making trainers out of used or cheap equipment that can be acquired in our lab or is a readily available item in order to produce an enhanced, high-yield learning experience at a low cost. Specifically, in creating the SALAD simulation system we were able to provide a simulation experience that has not been previously taught to our students in adjunct with the teaching of traditional intubation techniques at a much lower cost than purchasing a commercially available SALAD trainer. Ultimately, this extra training and simulation will help our students become better doctors to help their future patients without the burden of a high cost.
Limitations to this SALAD simulator include having to empty the suction canisters, a 2-gallon fluid restriction, and a space restriction because of the 54-gallon tote on all sides. Possible improvements to be considered include increasing the amount of fluid available by using a container larger than 2 gallons. Increasing the size of the suction canisters will decrease the frequency of emptying them, leading to more time being used to engage in simulations rather than tending to the simulator. Using a smaller container to hold the mannequin and collect the secretions not collected by suction could improve the space restriction, permit easier observation by students, and would encourage learning. Another limitation is that our SALAD system was based on an adult mannequin. Further development is required to see if a comparable pediatric version of our SALAD system can be made.
In addition, the SALAD simulator at our institution has so far only been used to train students who had zero prior experience with managing airways. While improvement in airway management skills was noted immediately after the training sessions in our institution’s Medical Simulation class, no data was gathered on long-term skill retention of the students who trained with this system. Further research would need to be conducted to confirm this. It is also not known if individuals with prior airway management experience would benefit from using this system. One possible solution is to increase the flow rate of fluid, which would increase the difficulty of the airway and provide more of a challenge. Again, further research would need to be conducted to see if those experienced with airway management would benefit from our SALAD system.
References
- Ducanto J, Serrano KD, Thompson RJ. Novel airway training tool that simulates vomiting: Suction-Assisted Laryngoscopy Assisted Decontamination (SALAD) System. West J Emerg Med. 2017;18(1):117-120. doi:10.5811/westjem.2016.9.30891.
- Kennedy CC, Cannon EK, Warner DO, et al. Advanced airway management simulation training in medical education: A systematic review and meta-analysis. Crit Care Med. 2014;42(1):169– 78. doi:10.1097/CCM.0b013e31829a721f.
- Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99(2):607–13. doi:10.1213/01.ANE.0000122825.04923.15.
- Khan K, Pattinson T, Sherwood M. Simulation in medical education. Med Teach. 2011;33(1):1-3. doi:10.3109/0142159X.2010.519412.
- Dias RD, Neto AS. Stress levels during emergency care: a comparison between reality and simulated scenarios. J Crit Care. 2016;33:8–13. doi:10.1016/j.jcrc.2016.02.010.
Appendix