Dhimitri A Nikolla, DO
Emergency Physician
AHN Saint Vincent, Erie PA
Introduction
Proning is a method of positioning hypoxemic patients to improve oxygenation. It reduces mortality in mechanically ventilated patients with severe Acute Respiratory Distress Syndrome (ARDS),1 and has been recommended for patients mechanically ventilated due to Coronavirus Disease 2019 (COVID-19) pneumonia caused by the severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2).2,3
Awake proning, or proning of non-intubated patients, has been piloted in the past for ARDS,4 but it has re-emerged as a critical intervention for COVID-19 pneumonia with hypoxemia.5-7
Purpose
COVID-19 pneumonia may present with severe hypoxemia requiring ventilatory support, but interventions such as noninvasive positive pressure ventilation (NIPPV) produce aerosols that carry significant risk of transmission to healthcare workers (HCWs).5,8 Early intubation has been advocated to limit aerosols and prevent worsening respiratory failure, but this strategy can quickly deplete critical care resources.5,6 Therefore, awake proning has emerged as an intervention to improve oxygenation in non-intubated COVID-19 pneumonia patients, because it requires few resources and does not produce aerosols.
Pathophysiology
Proning involves turning patients onto their chest/abdomen (Figure1). The primary mechanism by which it improves oxygenation is by decompressing and recruiting dorsal lung areas allowing for more uniform aeration of the lung tissue (Figure 2). Also, since pulmonary blood flow is normally directed to the dorsal lung regions and is minimally affected by gravity, proning allows for improved aeration of the better perfused dorsal lung tissue reducing shunting (Figure 2).9 This is the mechanism by which proning likely improves oxygenation in early COVID-19 pneumonia, by mitigating severe shunting.6,10
Evidence
Studies on awake proning in COVID-19 pneumonia are limited but promising.5-7 The largest is a case series of 50 adult emergency department patients capable of self-proning with documented SARS-CoV-2 infection who presented with SpO2 <90% and remained ≤93% despite supplemental O2. The median SpO2 was 80% (IQR 69-85) which improved to 84% (IQR 75-90) after supplemental O2 (non-rebreather mask or nasal cannula) which improved to 94% (IQR 90-95) after 5 minutes of awake proning.5 Although the evidence is limited, awake proning is a simple intervention that may provide significant benefit.
Procedure
Awake proning is most appropriate for hypoxemic patients with minimal or mild respiratory distress, sometimes described as “happy hypoxemics.”5 Reported exclusion criteria are primarily focused on worsening respiratory failure (Table 1).4
Protocols may include a sequence of positions (Figure 3) with a goal of 0.5-2 hours in each position, but patients may alter position based on comfort. They may remain non-supine for up to 16-18 hours daily. They may change positions on their own if they are capable, which may help limit exposure to HCWs.5,6 Awake proning can be performed in combination with supplemental O2, high flow oxygen, or NIPPV.4-6 Lastly, it is critical to closely monitor COVID-19 pneumonia patients during awake proning as their respiratory status can rapidly decompensate.5
Take Home Message
Awake proning is an emerging therapy for COVID-19 pneumonia with acute hypoxemic respiratory failure that can be utilized in the ED with few resources and can improve oxygenation without the risk of generating aerosols.
References
- Munshi L, Del Sorbo L, Adhikari NKJ, et al. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann Am Thorac Soc. 2017;14(Supplement_4):S280-s288.
- COVID-19 Treatment Guidelines Panel. Coronavirus Diseases 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. https://www.ncbi.nlm.nih.gov/pubmed/. Published 2020. Accessed May 8, 2020.
- Alhazzani W, Moller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit Care Med. 2020.
- Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020;24(1):28.
- Caputo ND, Strayer RJ, Levitan R. Early Self-Proning in Awake, Non-intubated Patients in the Emergency Department: A Single ED’s Experience during the COVID-19 Pandemic. Acad Emerg Med. 2020.
- Slessarev M, Cheng J, Ondrejicka M, Arntfield R, Critical Care Western Research G. Patient self-proning with high-flow nasal cannula improves oxygenation in COVID-19 pneumonia. In: Can J Anaesth. United States2020.
- Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. In: Ann Intensive Care. Vol 10. Germany2020:33.
- Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797.
- Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS With Prone Positioning. Chest. 2017;151(1):215-224.
- Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. Covid-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2020.
Figure 1 displays the prone position.
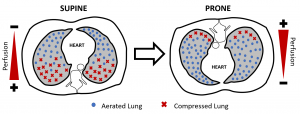
Figure 2 displays how compressed dorsal lung tissue in the supine position becomes aerated in the prone position while pulmonary blood flow remains directed to the dorsal lung tissue in both positions.
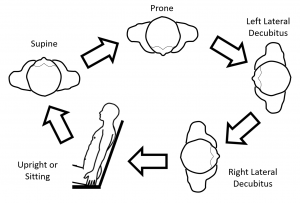
Figure 3 displays an example of a proning sequence where patients are asked to remain in each position for 0.5-2 hours each as tolerated.
Table 1 Suggested Contraindications to Awake Proning
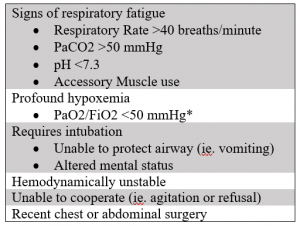
*Low SpO2 in the absence of significant respiratory distress or altered mental status may be well tolerated in some COVID-19 pneumonia patients.5
