John Oh, MD
Ashley Lauria, DO
Kent Hospital Emergency Medicine Residency
Introduction
This case describes a young male who presented to the Emergency Room (ER) with a chief complaint of sudden onset bilateral lower extremity paralysis. He was found to have thyrotoxic periodic paralysis (TPP), which is a subset of hypokalemic periodic paralysis. TPP occurs mainly in Asian males with decompensated hyperthyroidism. Among the Chinese and Japanese population, it occurs in 2% of patients with hyperthyroidism, in contrast to North America where there is a 0.1% incidence.1 It is hypothesized that the mechanism behind this phenomenon is an increase in activity of cellular Na-K ATpase and a mutation in Kir2.6, a potassium channel protein2.
History:
A 30-year-old Chinese American male presented to the ER via EMS with a chief complaint of leg weakness. Six hours prior to his presentation, he awoke from sleep with acute paralysis of the bilateral lower extremities. For one week leading up to the presentation, he had intermittent myalgias in the arms and legs, but denied weakness. He also described watery diarrhea for 1-2 days during a trip to China one month prior. The patient’s past medical history was significant for Grave’s disease, however he was no longer on medications. He denied weight change, heat intolerance, fatigue, hyperactivity, diaphoresis, swelling, dyspnea, palpitations, or recent illness.
Physical exam:
Vitals: Temp 98.0 HR 90 RR 12, BP 122/51, SPO2 96 RA
General: In bed awake, no acute distress, alert and oriented x3.
Neck: Supple, no goiter/thyromegaly
Pulmonary: Normal effort, clear to auscultation bilaterally
Cardiovascular: Regular rate and rhythm. S1 s2 present, no murmurs/rubs/gallops
Abdomen: Soft, nontender, nondistended, no masses, NABS
Neurologic Exam
Mental Status: Alert and oriented x4, fluent speech, no dysarthria
Cranial nerves: PERRL and 3 mm bilaterally, no nystagmus, EOMI, facial sensation intact, symmetric smile, 5/5 SCM and trap muscles
Motor: Normal tone and bulk for age, no fasciculations/atrophy. No pronator drift.
UE: 5/5 strength on flexion and extension of arms and shoulders, grip strength 5/5.
LE: Unable to engage hip flexors, unable to perform hip adduction/abduction, unable to perform knee flexion/extension, legs/hips unable to resist gravity (in summary, 1/5 strength). 3/5 dorsiflexion/plantar flexion.
Trunk: Apparent truncal weakness – unable to sit up in bed without using his arms to grab the rails. Is able to flex his abs.
Reflexes: Brachioradialis and biceps reflexes 2+, areflexic in the lower extremities throughout, Babinski sign absent.
Sensory: Mild diminished sensation to pain below knee, otherwise completely intact throughout
Coordination: Finger to nose intact bilaterally
Diagnostic results:
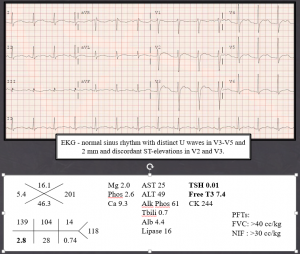
Figure 1: Diagnostic Results
ER course:
Shortly after presentation, the patient developed ascending weakness involving the truncal muscles; he needed to hold onto the bed rails to sit up in bed. The patient was administered oral potassium and transferred to the care of his endocrinologist at another facility. Follow up at one month revealed that the patient’s thyrotoxicosis was treated with intravenous propranolol and patient had regained full motor function within 24 hours. Chart review revealed that he had also had a similar presentation to an outside hospital in 2012, when he was diagnosed with TPP.
Thyrotoxic Periodic Paralysis:
Epidemiology
- Among the Chinese and Japanese population, it occurs in 2% of patients with hyperthyroidism, in contrast to North America where there is a 0.1% incidence
- Over 95 percent of thyrotoxic PP cases occur in men
- Peak in incidence 20 and 39 years of life
Symptoms
- Subacute onset lower extremity muscle weakness over 1-2 day
Mechanism
- Subset of hypokalemic periodic paralysis
- Mechanism of hypokalemia: thyroids hormones stimulate the Na+-K+ ATPases on cell membrane, leading to disproportionate efflux of Na+ outside of cells and influx of K+ into cells. As a result, the serum K+ falls.
- However, total body potassium is normal or even higher than normal, they are displaced into the intracellular space.
- In addition, a mutation to Kir2.6, a potassium channel protein, leads to further disproportionate influx of potassium into cells and out of the serum.
Diagnosis
- Hypokalemia and periodic paralysis in the setting of low TSH or high free T3 levels.
Treatment
- Treat hyperthyroidism acutely with propranolol (2 mg IV bid) and methimazole 20 mg daily
Slowly replete K (30 meq q4 hrs with max dose of 90 meq, oral) with frequent BMP to avoid rebound hyperkalemia
Discussion:
Hyperthyroidism is a fairly common condition that affects approximately 1.2% of the US population, and is therefore a well-studied phenomenon.3 Our patient however denied typical symptoms of hyperthyroidism, which include palpitations, heat intolerance, and weight loss.4 The only symptoms he reported from his thyrotoxicosis were generalized myalgia and lower extremity paralysis. Another remarkable finding was the patient’s hypokalemia, which was only moderate at 2.8. Further literature review reveals that in those with hyperthyroidism, the average potassium level seen in TPP is 2.0, based on a 10 year analysis of TPP in 135 patients.5 Most patients with TTP develop weakness primarily in the lower extremities, as seen in our case6. This case demonstrates that hyperthyroidism must be considered as a cause in focal weakness, and if not readily recognized, it can lead to dangerous arrhythmia as evidenced by EKG changes in the setting of moderate hypokalemia.
References
- Kung AW. Clinical review: thyrotoxic periodic paralysis: a diagnostic challenge. J Clin Endocrinol Metab (2006) 91(7):2490–5.10.1210/jc.2006-035
- Vijayakumar A, Ashwath G, Thimmappa D. Thyrotoxic periodic paralysis: clinical challenges. J Thyroid Res 2014; 2014:649502
- R. A. Nordyke, F. I. Gilbert Jr., and A. S. M. Harada, “Graves’ disease. Influence of age on clinical findings,” Archives of Internal Medicine, vol. 148, no. 3, pp. 626–631, 1988.
- Bahn RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. American Thyroid Association American Association of Clinical Endocrinologists. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract 2011;17: 456–520.
- Chang CC, Cheng CJ, Sung CC, et al. A 10-year analysis of thyrotoxic periodic paralysis in 135 patients: focus on symptomatology and precipitants. Eur J Endocrinol. 2013;169:529-36.
- Pompeo A, Nepa A, Maddestra M, Feliziani V, Genovesi N. Thyrotoxic hypokalemic periodic paralysis: An overlooked pathology in western countries. Eur J Intern Med. 2007;18:380–390
- Li J, Yang XB, Zhao Y. Thyrotoxic periodic paralysis in the Chinese population: clinical features in 45 cases. Exp Clin Endocrinol Diabetes. 2010;118:22-6.
- Pothiwala P, Levine SN. Analytic review: thyrotoxic periodic paralysis: a review. J Intensive Care Med 2010; 25:71.
- Chan A, Shinde R, Chow CC, et al. Hyperinsulinaemia and Na+, K(+)-ATPase activity in thyrotoxic periodic paralysis. Clin Endocrinol (Oxf) 1994; 41:213.
